A few weeks ago, we published a blog about the active substances commonly found in disinfectants and antiseptics. We mentioned that the efficacy of these substances against different microorganisms and how some microorganisms show resistance towards some compounds. Perhaps unsurprisingly, this is due to the cellular structure of the microorganism. Today, we would like to provide an insight into the structure of these microorganisms and how that contributes to their resistance towards disinfectants. Firstly, how does the resistance of these microorganisms rank? The diagram below shows an overview of the antimicrobial spectrum of disinfectants from the most resistant to least resistant microorganism.

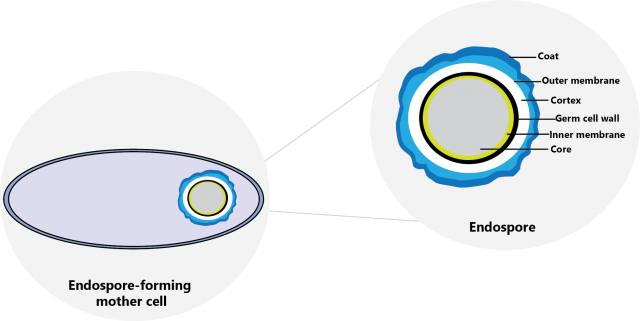
Bacterial Endospore
“The toughest player in the game.” — Spore-forming bacteria are known to be the toughest microorganism due to their ability to form a spore coat known as an endospore when under stress to protect themselves from dying. Some examples of spore-forming bacteria include Bacillus cereus, Bacillus subtilis, and Clostridium tetani. These endospores remain dormant until the environment is favorable to grow. Bacterial spores are resistant towards disinfectants containing only chlorhexidine, quaternary ammonium compounds, and phenolic compounds. On the contrary, disinfectants with sporicidal activity includes those containing peracetic acid, hydrogen peroxide, and chlorine compounds.
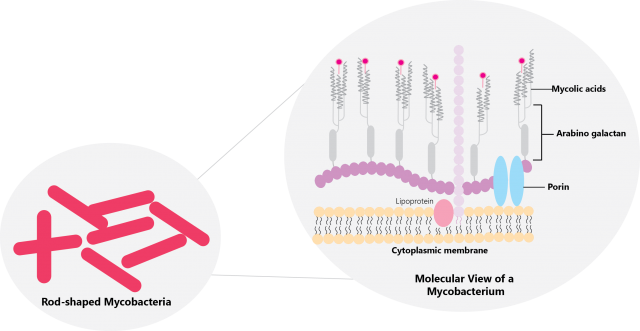
Mycobacteria
“Tuberculosis?” — Mycobacteria, or commonly referred to as acid-fast bacteria, are the second most resistant microorganism towards disinfectants. Aside having high molecular weight lipids, the similar complex cell wall structure in all mycobacteria allows it to form a strong protective barrier that prevents the penetration of disinfectants. The high lipid content of these cell wall causes an inability to allow the penetration water-soluble disinfectants . Disinfectants containing alcohol, phenolic compounds, hydrogen peroxide, peracetic acid, and glutaraldehyde are highly recommended to achieve a mycobactericidal activity.
Small Non-Enveloped Virus
“Fun size viruses ain’t fun.” — Small non-enveloped viruses such as norovirus and poliovirus are the most resistant virus groups in the hierarchy. Aside from measuring at less than 50 nm in size, these viruses are hard to kill with disinfectants due to the presence of a very resistant protein coat—a capsid—that requires denaturation.

Gram-Negative Bacteria
Stained pink from a Gram stain, Gram-negative bacteria has an envelope that consists of three layers: an outer membrane, a peptidoglycan cell wall, and an inner membrane layer. The lipopolysaccharide (LPS) composition and cation content present on the outer membrane of these Gram-negative bacteria contributes to the strength of the LPS-LPS links, creating a barrier with relatively smaller porins for disinfectants to pass through. Pseudomonas aeruginosa, Burkholderia cepacia, and Proteus spp. are some examples of Gram-negative bacteria that are resistant to certain active substances in disinfectant products.

Fungal Spores
“Mooooom! I see a mould spot!” — Fungal spores are quite different from bacterial spores. There are two groups of fungi, namely mould such as Aspergillus brasiliensis, and yeast such as Candida albicans. Mould and yeast acquire their intrinsic resistance due to the presence of a cell wall that acts as a barrier to prevent or reduce the entrance of disinfectants. Additionally, the chemical composition of a yeast cell affects the porosity of these cells and allows the modulation of disinfectants into these cells. The susceptibility of these pores are also affected by the age of the yeast culture. Disinfectants containing hydrogen peroxide, glutaraldehyde, iodophors, chlorine, and phenolic compounds are known to have fungicidal activity.

Large Non-Enveloped Virus
When compared to small non-enveloped viruses, a large non-enveloped virus measures from 50 nm to 100 nm in size. Adenovirus is an example of a large non-enveloped virus. The resistance of these viruses is lower compared to small non-enveloped viruses due to a larger surface area that increases the vulnerability of these viruses towards disinfectants.
Gram-Positive Bacteria
Stained purple from a Gram stain, the cell wall of Gram-positive bacteria—essentially being composed of peptidoglycan and teichoic acid—are not as effective in preventing the entry of disinfectants. The surviving rate of these bacteria are dependent to the growth rate and presence of growth-limiting nutrients as the thickness and peptidoglycan bonds will be altered, increasing the susceptibility of the bacteria to disinfectants. Disinfectants containing alcohol, quaternary ammonium compounds, and chlorhexidine exhibits bactericidal activity towards Gram-positive bacteria.

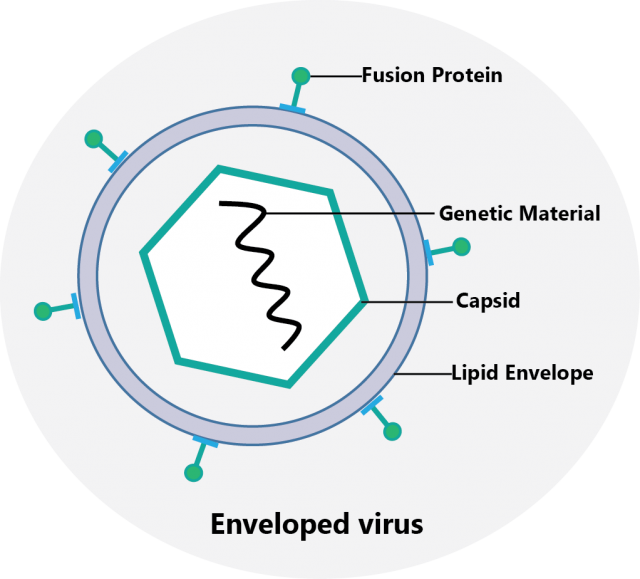
Enveloped Virus
Lipid enveloped viruses are the most susceptible group of microorganisms in the hierarchy. Human immunodeficiency virus (HIV), herpes virus, and coronavirus are examples of enveloped viruses. Viral fusion proteins on the lipid enveloped are compromised in the presence of disinfectants, thus decreasing the infectivity of enveloped viruses due to the loss of viral cell and host cell interaction. Disinfectants containing quaternary ammonium compounds, alcohols, and phenolic compounds exhibits virucidal activity towards enveloped viruses. We explained the differences between non-enveloped and enveloped viruses here and how it could affect the testing requirements of your disinfectant.
That brings us to the end to the hierarchy. Please note that resistance of these microorganisms may vary according to different studies and findings. If you require further assistance on which microorganism your product is effective against, do feel free to contact one of our experts today.
Reference:
1. Maillard, J.-Y. (2001). Virus Susceptibility to Biocides: An Understanding. Reviews in Medical Microbiology, 12(2), 63-74.
2. McDonnell. G & Russell, D.A. (1999). Antiseptics and Disinfectants: Activity, Action and Resistance. Clinical Microbiology Reviews, 12(1), 147-179.
3. Rossington, K. (2021). Virucidal Testing of Cleanroom Disinfectants. Retrieved from https://www.chemanager-online.com/en/restricted-files/215118

