“Everything in the room was positive—the walls, the bed, the doors, the curtains, the phones, the sinks, the whiteboard, the poles, the pump, the mattress, the bed rails, the canister holes, the window shades, the ceiling.”—Dr Scott Lorin, President of Mount Sinai Hospital, Brooklyn.
The above passage was written in 2019 by Matt Richtel and Andrew Jacobs in The New York Times on Candida auris, a mysterious infection indeed. If it wasn’t scary when Centers for Disease Control and Prevention (CDC) had reported this yeast species as an emerging global threat, Columbia Broadcasting System’s breaking news on the spread of this superbug in hospitals and long-term care facilities in Texas (22 cases) and Washington D.C. (101 cases) might have been the new Jason from Friday the 13th.
Superbug Candida auris
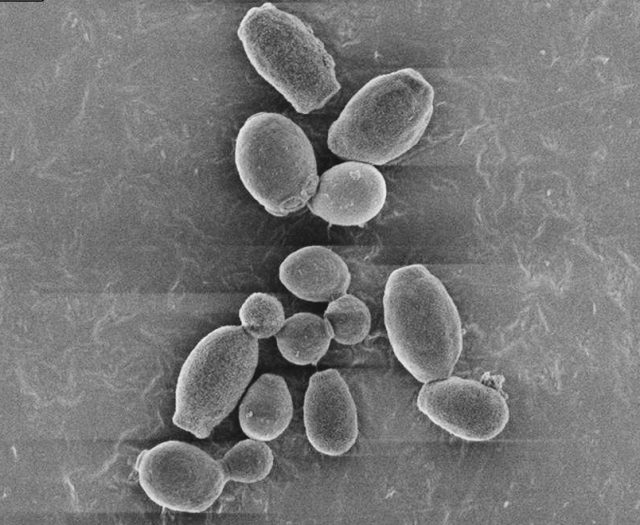
The diagram above shows a Scanning Electron Micrograph of Candida auris. Photo courtesy of Larkin et al. (2017)
“Get it off, get it off!”—Just like any other bugs, keep it far, far away from us. Superbugs were first discovered in 2016. By definition, superbugs are microorganisms such as bacteria, fungi, viruses, and more that are resistant to a large group of antibiotics and/or medication causing the kill rate of these harmful microorganisms to decrease. In a way, these superbugs do have superpowers: immortality that makes them difficult to treat. Since 2019, Candida auris has been the new kid on the block.
Closely related to Candida albicans, C. auris was first discovered in 2009 in Japan. It is a multidrug-resistant yeast species that causes invasive infections in blood, wounds, and in the ear. These infections occur most commonly amongst hospitalized patients with a weakened immune system. This highly transmissible yeast is transmitted through contact and survives persistently on hard surfaces in hospitals and other healthcare settings.
The Resistance Profile of Candida auris
“Look! Up in the sky! It’s a bird! It’s a plane! It’s Superman!”—A complete opposite of Superman, but a probable villain lurking in hospitals, Candida auris was named a superbug due to its resistant towards multiple antifungal medications. There are three major classes of antifungal medications commonly used in treating yeast or fungal infections namely triazole, polyene, and echinocandin. Amongst the 101 cases isolated in Washington D.C., three Candida auris strains were pan-resistant—a resistant to all classes of antifungal medication. This finding is not new, as its pan-resistance have been reported in January 2020 in CDC’s Morbidity and Mortality Weekly Report (MMWR) of positive infections in New York from the year 2016 to 2019. Fast forward to a year later, CDC’s recent MMWR had reported Candida auris to be 85% resistant towards class azoles, 33% towards amphotericin B (class polyene) and 1% towards echinocandin. Is it just me or did you get goosebumps too?
How to Prevent the Transmission of Candida auris?
As you’re familiar with, Candida auris is transmitted through contact. The first step in preventing the spread of this superbug begins with us whether you’re a healthcare professional or a visitor in the hospital. It is utmost important to wash your hands thoroughly with soap and disinfect your hands before and after touching a patient with a Candida auris infection or the surroundings of their room. Dr Scott Lorin was not wrong when he said it was everywhere.
As a disinfectant testing laboratory, we would like to emphasize on choosing the right disinfectant whether for your hands or environmental disinfection. Despite being effective against Candida albicans, some disinfectants may not be effective towards Candida auris. According to List P of the United States Environmental Protection Agency (EPA), here are some examples active substances that have been approved to be effective against Candida auris:
- Hydrogen peroxide
- Peracetic acid
- Octoanoic acid
- Dodecylbenzenesulfonic acid
- Sodium Hypochlorite
- Isopropyl Alcohol
- Sodium dichloro-s-triazinetrione
- Ethanol
Please note that these active substances are listed as individual ingredients; specific formulation and/or combinations may be required to prove effective against Candida auris. According to a study conducted by Rutala et al. (2019), disinfectants with a combination of alcohol and quaternary ammonium compounds had also shown effective against Candida auris.
Have a quick read here to learn more on other factors to consider when choosing the right disinfectant.
How to Evaluate the Efficacy of Your Disinfectant against Candida auris?
“Hey Zabel, how can I market my disinfectant with the claim “Effective against Candida auris?”—We’d advise Zabel’s friend to have Phase 2, Step 1 and, where applicable, Phase 2, Step 2 efficacy test reports to support his product claim. TECOLAB has a variety of antibiotic-resistant microorganism in our microorganism library including Candida auris for you to pick. Disinfectant manufacturers can choose to test the efficacy of this superbug according to the standards listed in table below.
| DISINFECTANTS IN THE MEDICAL AREA | TEST REQUIRED | |
| PHASE 2, STEP 1 | PHASE 2, STEP 2 | |
| Hygienic handrub | EN 13624 | *** |
| Hygienic handwash | ||
| Surgical handrub or handwash | ||
| Surface disinfectant with wiping action | EN 13624 | EN 16615 |
| Surface disinfectant without wiping action | EN 13697 | |
| Airborne disinfection system | *** | EN 17272 |
| Instrument disinfectant | EN 13624 | EN 14562 |
| *** No relevant standards currently available | ||
“Hey Zabel, our competitors have had the same efficacy tests done for surface disinfectant. What could make our product stand out?”—Apart from proving effectiveness against Candida auris, evaluating the residual efficacy of your product towards this superbug could promote product uniqueness amongst others sold in the market. TECOLAB evaluates surface disinfectant residual efficacy on non-porous surfaces against Candida auris according to Publicly Available Specification (PAS) 2424.
Not sure where to start with your product claim against this superbug? Let us assist you step-by-step by providing a cost-effective efficacy test plan and consultation to kick start your journey with us! Contact us here to speak to one of our experts today.
Reference:
1. Centers for Disease Control and Prevention. (2021). Candida auris. Retrieved from https://www.cdc.gov/fungal/candida-auris/index.html
2. Centers for Disease Control and Prevention. (2021). Infection Prevention and Control for Candida auris. Retrieved from https://www.cdc.gov/fungal/candida-auris/c-auris-infection-control.html#dis-references
3. Lyman, M., Forsberg, K., Reuben, J., Dang, T., Free, R., Seagle, E.E., Sexton, J., Soda, E., Jones, H., Hawkins, D., Anderson, A., Bassett, J., Lockhart, S.R., Merengwa, E., Iyengar, P., Jackson, B.R. & Chiller, T. (2021). Notes from the Field: Transmission of Pan-Resistant and Echinocandin – Resistant Candida auris in Health Care Facilities – Texas and the District of Columbia, January – April 2021. Centers for Disease Control and Prevention. Retrieved from https://www.cdc.gov/mmwr/volumes/70/wr/mm7029a2.htm?s_cid=mm7029a2_w
4. Ostrowsky, B., Greenko, J., Adams, E., Quinn, M., O’Brien, B., Chaturvedi, V., Berkow, E., Vallabhaneni, S., Forsberg, K., Chaturvedi, S., Lutterloh, E. & Blog, D. (2020). Candida auris Isolates Resistant to Three Classes of Antifungal Medications – New York, 2019. Centers for Disease Control and Prevention. Retrieved from https://www.cdc.gov/mmwr/volumes/69/wr/mm6901a2.htm?s_cid=mm6901a2_w
5. Rutala, W. A., Kanamori, H., Gergen, M. F., Sickbert-Bennett, E. E., & Weber, D. J. (2019). Susceptibility of Candida auris and Candida albicans to 21 germicides used in healthcare facilities. Infection Control & Hospital Epidemiology, 40(3), 380–382.
6. United States Environmental Protection Agency. (2021). List P: Antimicrobial Products Registered with EPA for Claims Against Candida Auris. Retrieved from https://www.epa.gov/pesticide-registration/list-p-antimicrobial-products-registered-epa-claims-against-candida-auris

